Top tips to support your Immune System
We’re reaching that time of year when colds and coughs are circulating. With more than 200 different common cold viruses you’d be forgiven for thinking that catching one is inevitable but I have some top tips for you to help fight them off.
My first tip is probably not one you’d expect – I’m not talking about vitamin tablets or superfood powders – I’m talking about your gut!
Did you know that more than 70% of your immune system is based in your gut? Research has shown that it’s possible to reduce the frequency of catching coughs and colds by supporting the beneficial bacteria that live there. This is often my first step with clients who come to me seeking advice on boosting their immune system. Luckily, there are lots of simple ways you can keep your gut happy.
Gut bacteria thrive on fibre, so increasing your intake of fruit and vegetables is an easy way to help them. Aim for five a day – more if you can, (one portion is about 80 grams) and try to ‘eat a rainbow’. Just as we have different preferences so do different strains of bacteria, so eating a wide variety is the best way to ensure that each strain is getting what they need. Another way to pack more fibre into your diet is to swap refined carbohydrates for complex carbohydrates – choose brown pasta and grains over the white varieties which are much lower in fibre and nutrients.
Another way to support your gut health so that it can keep your immune system working effectively is to try fermented foods. These are foods that contain live bacteria to populate the gut – sometimes referred to as ‘probiotic’ foods. Unsweetened, natural live yoghurt, milk or water kefir, kombucha, sauerkraut, kimchi and miso are all examples of fermented foods and most can be found in large supermarkets or your local health food store. You could try adding some natural yoghurt or kefir to some granola and berries for breakfast, or sip on some warm miso as a comforting drink (don’t make the miso too hot or it will kill off the bacteria).
Vitamin C is claimed to be another well-known cold remedy and at this time of year there are adverts for high-street or supermarket own brand supplements everywhere. Interestingly, the evidence behind these claims is weak. There is limited evidence to suggest that vitamin C can actually prevent a cold, and only slightly more to suggest it can reduce the duration and severity of symptoms. My advice would be to steer clear of vitamin C supplements (check out my blog post on supplements for more reasons!) but to include fruit and vegetables rich in it instead – dark leafy greens are an excellent source and the wide variety of other nutrients in them will help you much more than the fillers in the cheap supplements!
Finally, zinc – another well-known ‘anti-cold’ nutrient. The evidence here is a little stronger but again inconclusive – and also stronger in terms of reducing duration and severity, rather than prevention. Foods to include to ensure you’re getting enough zinc are meat and shellfish or legumes, nuts and seeds for the vegetarians and vegans out there.
There are of course specific foods that are traditionally used for fighting coughs and colds, such as chicken soup, garlic and ginger. I’ll save these for another blog post so keep checking back.
In the mean time, wrap up warm, eat your vegetables and stay healthy! X
Gut bacteria
In Ancient Greece, Hippocrates believed that all diseases start in the gut. Thousands of years later and it looks like he had a point. More and more evidence is emerging that points to the pivotal role of the gut in health and disease and at gut bacteria (the microbiome) in particular.
We each have trillions of bacteria living in our gut, taking up residence from the moment we are born (some research suggests they might even start colonising before birth) and changing throughout our life span, influenced by everything from diet to medication, stress and trauma and even lifestyle choices.1 So far, research has shown that these bacteria can have a great effect on maintaining the mucosal barrier in the gut (to stop bad guys getting out into the bloodstream and wreaking havoc)1, extracting nutrients and energy from food (it has even been suggested that obese individuals have bacteria that is especially adept at this)2, and in immunity – 70% of your immune system is actually in your gut!1 Evidence also shows a gut-brain connection, and there is a link between disturbance of gut bacteria and mood, with one study alleging 60% of anxiety and depression patients had bacterial imbalance.3 Much more research is needed but the implications for our health are really exciting.
An aspect of gut bacteria that I see most commonly in clinic is something called ‘dysbiosis.’ This is when beneficial bacteria and less beneficial bacteria become imbalanced.4 Symptoms are incredibly varied, ranging from IBS type symptoms, tummy aches, flatulence, abdominal discomfort, irregular bowel habits, to symptoms that you might not think could be connected to the gut – for example fatigue, aches and pains, anxiety, depression. Dysbiosis is something I often look to address first, before moving on to look at a client’s other imbalances, because if the gut isn’t working optimally it can be very difficult to adequately process and absorb all the nutrients needed to keep the rest of the body functioning optimally.
The great news is that we can use diet to keep our gut bacteria happy, and here are some ideas you can try:
- Gut bacteria love veggies, and they love variety! So try to eat a rainbow everyday – orange, red, purple, white, green veggies. Not only will you reap the benefits of a variety of antioxidants, polyphenols and phytonutrients but you’ll also be getting a healthy dose of fibre. Fibre helps your bacteria thrive.5
- Fermented foods: natural yoghurt, kefir, kombucha, sauerkraut, miso, kimchi, apple cider vinegar, fermented pickles, tempeh, unpasteurized cheese. These contain bacteria that can help to colonize your gut with the good guys. (Top tip – always buy fermented foods that have to live in your fridge. If it’s a store-cupboard item, it probably doesn’t have enough bacteria. For example, most supermarket pickles will not be fermented – you’d have better luck at a health food shop. You could also try making them yourself.)6
- Reducing processed foods and alcohol. These are bad news for the gut, suppressing good bacteria and feeding the bad guys.7
- Don’t take antibiotics unless your GP tells you they’re necessary. Antibiotics flush out all bacteria – good and bad. Interestingly, a recent study suggests that the microbiome recovers more quickly than previously thought from a course of antibiotics, but several key beneficial strains of bacteria take slightly longer.8 If you have had to take antibiotics, try to gradually reintroduce bacteria.
- Lifestyle – stress, lack of sleep and lack of exercise have all been linked to a reduction in the diversity of gut bacteria. Try to relax, get enough shut-eye and exercise regularly.9
It’s important to take it slow when introducing more fibre or fermented foods into your diet. Adding too much too soon can result in more digestive symptoms – particularly abdominal discomfort and wind. It is also possible to take probiotic supplements, which can be really helpful for certain individuals. I would always suggest trying a ‘food-first’ approach – get as much as you can from your diet before turning to supplements.
References
- Thursby, E. and Juge, N. (2017). Introduction to the human gut microbiota. Biochemical Journal, 474(11), pp.1823-1836.
- Castaner, O., Goday, A., Park, Y., Lee, S., Magkos, F., Shiow, S. and Schröder, H. (2018). The Gut Microbiome Profile in Obesity: A Systematic Review. International Journal of Endocrinology, 2018, pp.1-9.
- Liu, L. and Zhu, G. (2018). Gut–Brain Axis and Mood Disorder. Frontiers in Psychiatry, 9.
- Hooks, K. and O’Malley, M. (2017). Dysbiosis and Its Discontents. mBio, 8(5).
- Hiel, S., Bindels, L., Pachikian, B., Kalala, G., Broers, V., Zamariola, G., Chang, B., Kambashi, B., Rodriguez, J., Cani, P., Neyrinck, A., Thissen, J., Luminet, O., Bindelle, J. and Delzenne, N. (2019). Effects of a diet based on inulin-rich vegetables on gut health and nutritional behavior in healthy humans. The American Journal of Clinical Nutrition, 109(6), pp.1683-1695.
- Rezac, S., Kok, C., Heermann, M. and Hutkins, R. (2018). Fermented Foods as a Dietary Source of Live Organisms. Frontiers in Microbiology, 9.
- Zinöcker, M. and Lindseth, I. (2018). The Western Diet–Microbiome-Host Interaction and Its Role in Metabolic Disease. Nutrients, 10(3), p.365.
- Palleja, A., Mikkelsen, K., Forslund, S., Kashani, A., Allin, K., Nielsen, T., Hansen, T., Liang, S., Feng, Q., Zhang, C., Pyl, P., Coelho, L., Yang, H., Wang, J., Typas, A., Nielsen, M., Nielsen, H., Bork, P., Wang, J., Vilsbøll, T., Hansen, T., Knop, F., Arumugam, M. and Pedersen, O. (2018). Recovery of gut microbiota of healthy adults following antibiotic exposure. Nature Microbiology, 3(11), pp.1255-1265.
- Conlon, M. and Bird, A. (2014). The Impact of Diet and Lifestyle on Gut Microbiota and Human Health. Nutrients, 7(1), pp.17-44.
Poo Taboo
People don’t talk about poo. It’s considered ‘bad taste,’ or ‘immature.’ Yet it can be one of the most useful indicators about what is going on in the body – the shape, size, colour and consistency alone can give us lots of clues and a useful tool I use in clinic to get the conversation rolling is the Bristol Stool Chart. Yes, if you come and see me, you can expect me to bring out a laminated sheet displaying different drawings of poo!
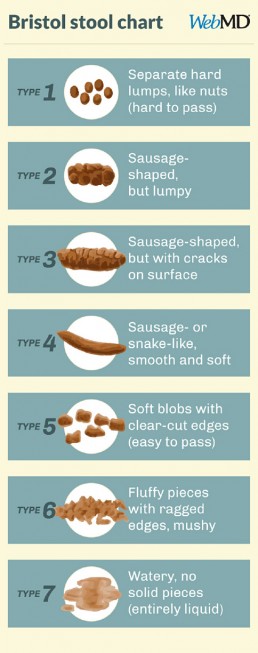
Generally speaking, types 3 and 4 are the ‘optimum’ stools, and you’d want to be producing them between 1-3 times most days. They should be easy to pass and painless, and not associated with any immediate urgency – i.e. if you have to wait until you find a loo it wouldn’t be uncomfortable. I say ‘generally’ because we are all different and there might be cases when an individual’s bowel habits don’t conform to the ‘optimum’ but are still perfectly healthy for them.
It’s also quite normal for stools to vary depending on what you’ve been eating most recently or how your lifestyle has been. For instance, have you ever been on holiday and not pooped for several days? Believe it or not, change in routine can really disrupt your loo schedule! Stress, medication, alcohol, indulgent meals, the menstrual cycle and illness can all impact and alter bowel movements but if you’re regularly experiencing constipation or urgency and loose stools, it might be a good idea to talk to someone.
Let’s look at the stool chart in more detail.
Types 1 and 2 are likely to go hand in hand with less frequent trips to the loo, or even with constipation. It might be that you’re dehydrated and need a bit more water – the body will draw water back out from the colon in order to compensate for the dehydration, making stools firmer and harder to pass. It might be that your fibre intake is low – these stools might be expected if you’re following a diet low in carbohydrates. It can even be a sign that you’ve been inactive – exercise can help to get things moving. These stools will have spent longer in the colon than is ideal, allowing for the reabsorption of toxins that should have been eliminated, including excess hormones. This is one reason why addressing bowel movements is a key part of supporting detoxification.
Types 5, 6, and 7 are likely to be more frequent, possibly associated with an urgency to go. It is likely that the stool has spent less time in the colon, therefore leaving less opportunity for food and water to be absorbed which is why these stools are looser, possibly indicating diaorrhea. Since less water is being absorbed, it is important to drink plenty of fluids in order to replenish. These types might also be indicative of a low fibre diet, since the stools are not firm.
Other aspects of appearance such as colour and greasiness, along with smell, are also useful indicators of what else might be going in in the gut. An ‘ideal’ poo (again, we’re speaking generally here) might be a mid-dark brown, wouldn’t leave marks on the toilet bowl and wouldn’t have a strong odour.
If you’d like to find out more about what your bowel movements might mean, please do get in touch and we can discuss how to optimize your digestion. There are even functional tests that can be done where a sample of your stool is sent to a laboratory to find out all sorts of more detailed information such as the composition of the bacteria in the gut, the level of enzymes that help to digest protein, carbohydrate and fats, whether there is any inflammation in the gut and even whether there are any yeast, microbes or parasites present. I’m very happy to break to poo taboo and get talking!
REFERENCES
Blake, M., Raker, J. and Whelan, K. (2016). Validity and reliability of the Bristol Stool Form Scale in healthy adults and patients with diarrhoea-predominant irritable bowel syndrome. Alimentary Pharmacology & Therapeutics, 44(7), pp.693-703.
Chang, Y., El-Zaatari, M. and Kao, J. (2014). Does stress induce bowel dysfunction?. Expert Review of Gastroenterology & Hepatology, 8(6), pp.583-585.
WebMD. (2019). What Kind of Poop Do I Have?. [online] Available at: https://www.webmd.com/digestive-disorders/poop-chart-bristol-stool-scale [Accessed 6 Aug. 2019].
Blood Glucose - The key to sustained energy
Ever heard of ‘food coma’? Ever had that post-lunch energy slump? Ever been ravenous mid-morning even though you had a big brekky? Chances are your blood glucose isn’t balanced. It’s one of the most common things I see in clinic and is often the starting point for my nutrition plans because without balanced blood glucose, it’s very difficult to bring everything else in the body into balance as well.
What is ‘blood glucose’?
When you eat, food gets broken down as it travels through the digestive system. As a result of this, the sugars (glucose) from foods are released into the blood stream. When this happens, a hormone called insulin is released from the pancreas (a large gland that sits behind the stomach). Insulin’s job is to encourage the cells in the body to let glucose in, where it will be used for energy. As the amount of glucose entering the blood stream falls, so does the level of insulin.
If too much glucose is released into the bloodstream, more insulin is released from the pancreas. It then stores the excess glucose in the liver, which will release it when more glucose is needed by the body – for example during exercise or between meals. This is supposed to be a good thing, making sure that your body has sustained energy.
When does blood glucose become imbalanced?
Different foods will have different effects on blood glucose – particularly depending on the protein, fat and fibre contents. But in simplistic terms, foods high in refined carbohydrate and sugars will cause a quicker and sharper spike in blood glucose. This leads to a quicker release and higher volume of insulin which will then lead to a quicker and sharper fall in the level of glucose in the blood. We refer to this as the ‘blood glucose rollercoaster.’
What does this actually mean?
These peaks and lows in blood glucose levels will result in peaks and crashes in energy – in other words, that mid-afternoon energy slump or that post-dinner ‘food coma.’ They’ll also make you hungry shortly after eating, irritable, possibly dizzy, have difficulty focusing and that dreaded feeling of hanger.
If blood glucose becomes dysregulated long-term, the knock-on effects can be widespread because insulin can interact with various other hormonal systems in the body. It is implicated in the balance of sex hormones and therefore plays a role in conditions such as endometriosis and PCOS, as well as PMS. It can affect hormones that relate to mood and stress. It can be linked to systemic inflammation and sleep disorders.
How to balance blood glucose?
The good news is that it’s actually relatively easy to balance blood glucose through your diet. Including plenty of fibre, protein, healthy fats and complex carbohydrates whilst reducing your intake of processed and refined carbohydrate foods. If you’re interested in finding out more please do get in touch with me at laura@lmnutrition.co.uk




